Don't Overlook These Critical Early Signs of Heart Disease
That question is an important one, because the earliest signs of heart disease often don't feel like a "heart problem" at all. Many are subtle and easy to dismiss—like unusual fatigue, shortness of breath, or even jaw pain.
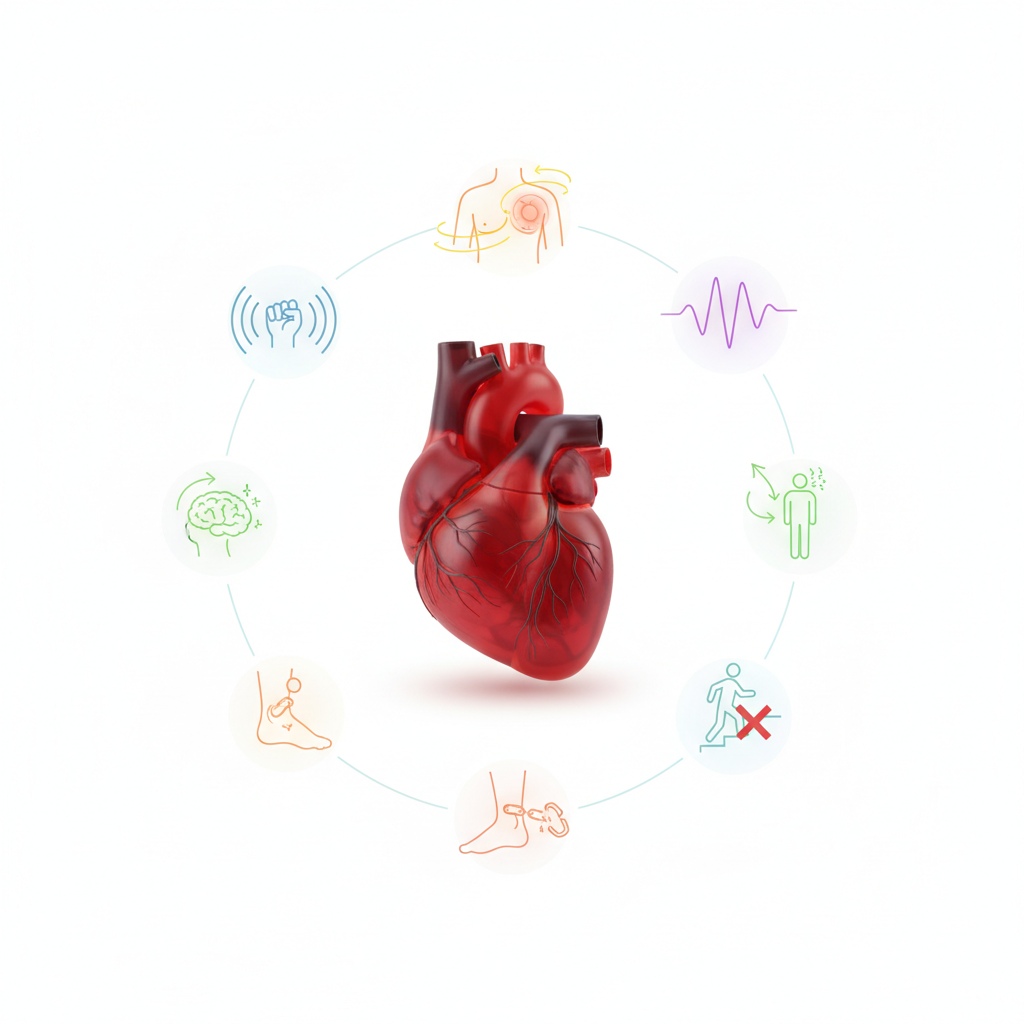
10 Early Warning Signs of Heart Disease You Shouldn't Ignore
Heart disease is often called a "silent killer" because its symptoms can be subtle and easily dismissed. Many people associate heart problems with sudden, crushing chest pain, but the reality is often much different. The earliest warning signs can be vague, intermittent, and mistaken for less serious issues like indigestion, muscle strain, or fatigue. Recognizing these signals is the first and most crucial step toward seeking timely medical care, which can make all the difference in preventing a major cardiac event. Paying attention to what your body is telling you is not about being paranoid; it's about being proactive with your health.
Key Warning Signs of Potential Heart Issues
1. Chest Discomfort (Angina)
While the classic image of a heart attack involves intense chest pain, the most common early sign is actually discomfort. This isn't always a sharp, stabbing pain. More often, it feels like pressure, squeezing, fullness, or a dull ache in the center of the chest. This sensation, known as angina, occurs when the heart muscle isn't getting enough oxygen-rich blood. The feeling may last for more than a few minutes, or it might come and go. It can be triggered by physical exertion or emotional stress and typically subsides with rest.
Many people mistake this discomfort for heartburn or indigestion, especially if it's mild. However, if the feeling is new, worsens, or occurs with minimal activity, it's a significant red flag. It's crucial not to dismiss any unusual chest sensation, as it is the most direct signal from your heart that something might be wrong.
2. Pain Radiating to Other Areas
Heart-related pain is not always confined to the chest. A classic sign is discomfort that starts in the chest and spreads to other parts of the upper body. Most commonly, this pain radiates down the left arm, but it can also affect the right arm, both arms, the back, neck, jaw, or even the stomach. This happens because the nerves from the heart and these other body parts send signals to the brain through the same pathways, and the brain can get confused about the source of the pain.
If you experience unexplained aches in these areas, especially if they accompany chest discomfort or are triggered by exertion, it warrants immediate attention. Pain in the jaw or back, in particular, is a symptom that is more frequently reported by women experiencing heart issues and is often overlooked.
3. Shortness of Breath (Dyspnea)
Feeling winded after climbing several flights of stairs is normal. However, experiencing shortness of breath after minimal exertion, like walking to your car or even while at rest, is a significant warning sign. This condition, medically known as dyspnea, can occur when the heart is unable to pump blood efficiently enough to deliver oxygen to the rest of the body. As a result, the lungs have to work harder, making you feel breathless.
This symptom can occur with or without accompanying chest discomfort. Sometimes, people find they can't breathe comfortably when lying down and have to prop themselves up with pillows to sleep. If you notice a new or worsening pattern of breathlessness that doesn't align with your fitness level, it's a strong indicator that your heart or lungs need to be checked.
4. Unexplained Fatigue or Weakness
Feeling unusually tired to the point where it interferes with your daily activities can be an early symptom of heart trouble. This isn't just the tiredness you feel after a long day; it's a profound, persistent exhaustion. This fatigue occurs when the heart can't pump enough blood to meet the body's needs. To compensate, the body diverts blood away from less vital organs, like the muscles in your limbs, and sends it to the heart and brain, leading to a feeling of overwhelming weakness and exhaustion.
This symptom can appear weeks or even months before a heart attack. If you suddenly feel drained by simple tasks that you used to handle easily, such as grocery shopping or walking up a small incline, and this fatigue doesn't improve with rest, it’s a clear signal to consult a doctor.
5. Dizziness or Lightheadedness
Feeling dizzy, lightheaded, or like you're about to faint can be a sign that your brain isn't receiving enough blood. While this can be caused by many things, including dehydration or standing up too quickly, it can also be linked to heart problems. A drop in blood pressure caused by a heart that isn't pumping properly or an abnormal heart rhythm (arrhythmia) can lead to these sensations. If dizziness is accompanied by chest discomfort or shortness of breath, the urgency to seek medical help increases significantly.
6. Swelling in Legs, Ankles, or Feet (Edema)
When your heart isn't pumping blood effectively, blood flow can slow down and back up in the veins in your legs. This pressure buildup can force fluid out of the blood vessels and into the surrounding tissues, causing noticeable swelling, a condition known as edema. This swelling is often most prominent in the feet, ankles, and legs. You might notice that your shoes feel tighter or see indentations left on your skin after you take your socks off. While leg swelling can have other causes, when it's related to the heart, it's a sign of congestive heart failure and should never be ignored.
7. Irregular Heartbeat (Arrhythmia)
It's normal for your heart to race when you're excited or nervous or to skip a beat occasionally. However, if you frequently feel like your heart is beating too fast, too slow, or is fluttering and skipping beats for more than a few seconds, it could be a sign of an arrhythmia. An arrhythmia is an irregular heartbeat that can be a symptom of underlying heart disease. While many arrhythmias are harmless, some can be serious and increase the risk of stroke or heart failure. Pay attention to feelings of "palpitations" or a "pounding" in your chest, especially if they occur with other symptoms like dizziness or weakness.
8. Nausea, Indigestion, or Stomach Pain
Sometimes, the symptoms of a heart attack can feel more like a stomach problem than a heart problem. Nausea, indigestion, heartburn, or abdominal pain can all be signs of a heart attack, particularly in women. This occurs because the nerves of the stomach and heart are located close together. If you experience these digestive-like symptoms, especially if they are not related to food you've eaten and are combined with other signs like sweating, lightheadedness, or chest discomfort, it's vital to consider the possibility of a cardiac event.
9. Breaking Out in a Cold Sweat
Sweating more than usual, especially when you are not exercising or in a hot environment, can be a warning sign. If you suddenly break out in a cold, clammy sweat for no apparent reason, it can signal a heart attack. During a cardiac event, your nervous system goes into "fight or flight" mode, which can trigger this type of sweating as your body tries to cool itself down under stress.
10. Persistent Coughing or Wheezing
A long-lasting cough or wheezing that produces white or pink-tinged mucus could be a sign of heart failure. This happens when the heart can't keep up with the body's demands, causing blood to back up in the blood vessels of the lungs. This congestion leads to fluid leaking into the lungs, resulting in a persistent cough that is similar to what someone with asthma or a lung infection might experience. If you have a cough that doesn't go away and is accompanied by shortness of breath or leg swelling, your heart could be the cause.
The Root Cause: Understanding Atherosclerosis
Many of these warning signs are a direct result of a process called atherosclerosis. This is a condition where plaque—a waxy substance made of cholesterol, fat, calcium, and other materials—builds up inside your arteries. Arteries are the blood vessels responsible for carrying oxygen-rich blood from your heart to the rest of your body. When plaque accumulates, it causes the arteries to narrow and harden, restricting blood flow.
This process can happen slowly over many decades, often starting in childhood. Initially, it produces no symptoms. However, as the blockage becomes more severe, it can lead to angina (chest discomfort) when the heart's demand for oxygen exceeds the restricted supply. The real danger occurs when a piece of this plaque ruptures. The body responds by forming a blood clot at the site of the rupture, which can completely block the artery. If this happens in a coronary artery supplying the heart muscle, it causes a heart attack. If it happens in an artery leading to the brain, it causes a stroke.
Common Questions About Heart Health
What are the key risk factors for heart disease?
Understanding your risk factors is just as important as recognizing symptoms. Some risk factors are beyond your control, while others can be managed through lifestyle changes or medication. Uncontrollable risk factors include age (risk increases as you get older), gender (men are generally at higher risk, but women's risk increases after menopause), and family history (a close relative with early heart disease). These genetic and age-related factors mean you need to be extra vigilant.
However, there are many major risk factors you can control. These include high blood pressure (hypertension), high cholesterol, and diabetes. Lifestyle factors also play a huge role. Smoking, a sedentary lifestyle, being overweight or obese, and a diet high in saturated fats, trans fats, and sodium all significantly increase your risk of developing atherosclerosis and subsequent heart disease. Managing these controllable factors is the most powerful tool you have for prevention.
How is heart disease diagnosed?
If you present to a doctor with potential symptoms, they will begin a diagnostic process to determine the health of your heart. This usually starts with a physical exam and a detailed discussion of your symptoms, medical history, and family history. The doctor will listen to your heart, check your blood pressure, and may order blood tests to check for levels of cholesterol, sugar, and certain proteins that can indicate heart damage.
From there, one of the most common initial tests is an electrocardiogram (ECG or EKG), which records the electrical activity of your heart to detect irregular rhythms or signs of a past or current heart attack. For a deeper look, a doctor might order an echocardiogram (an ultrasound of the heart), a stress test (monitoring your heart while you exercise), or a CT scan to look for calcium buildup in your arteries. In more advanced cases, a cardiac catheterization or angiogram may be necessary to get a direct look at the arteries and identify any blockages.
Conclusion
The early signs of heart disease are your body's way of sending an alarm. Ignoring them can have life-threatening consequences. While symptoms like chest pain, shortness of breath, and radiating discomfort are classic indicators, it's also important to pay attention to more subtle signs like unexplained fatigue, nausea, and swelling. Understanding the underlying causes like atherosclerosis and being aware of your personal risk factors can empower you to take control of your cardiovascular health. If you experience any of these warning signs, especially if they are new, persistent, or occur in combination, do not wait. Seeking a professional medical evaluation is the safest and most important step you can take.