Exploring the Factors That Cause HPV to Activate
It's a common and valid question: if HPV can lay dormant for years, what suddenly causes it to become active? The answer isn't a single event, but rather a combination of factors that can weaken your body's natural defenses.
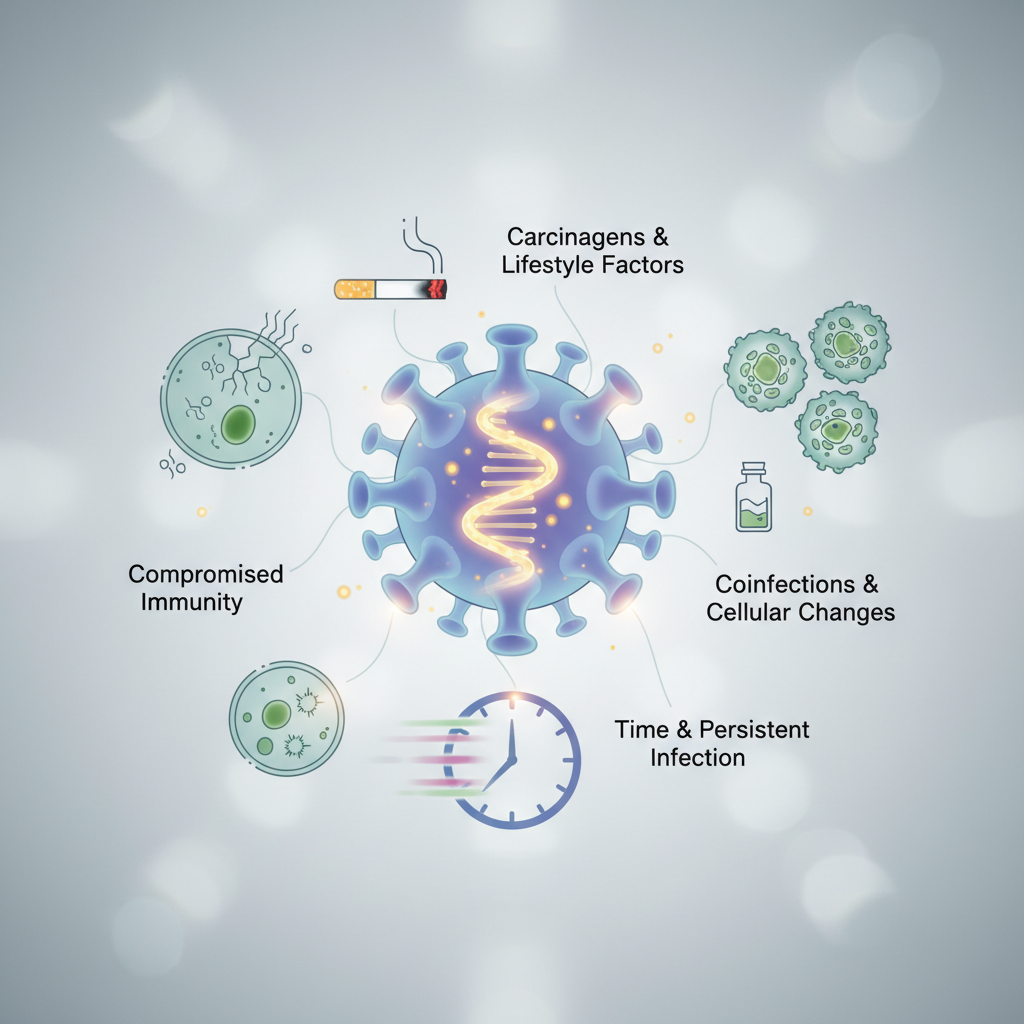
Key Factors That Can Trigger HPV Activation
Human Papillomavirus (HPV) is an incredibly common virus that most sexually active people will contract at some point in their lives. In the majority of cases, the body's immune system clears the infection on its own, often without the person ever knowing they had it. However, sometimes the virus doesn't fully clear and instead enters a dormant or "latent" state within the body's cells. It can remain this way for months, years, or even decades without causing any problems. The activation, or reactivation, of this dormant virus is what leads to health issues like genital warts or cellular changes that can lead to cancer. Understanding what triggers this activation is key to managing health and reducing risk.
The primary driver behind HPV activation is a change in the body's immune response. When the immune system is strong and vigilant, it keeps the latent virus in check. When it's weakened or compromised, it loses its ability to suppress the virus, giving HPV an opportunity to replicate and become active. Several factors, ranging from lifestyle choices to physiological changes, can influence this delicate balance.
A Weakened or Suppressed Immune System
This is the most significant factor influencing HPV activation. A robust immune system is the body's frontline defense, actively identifying and controlling viral invaders. When this system is compromised, its surveillance capabilities are diminished. This can happen for various reasons, including underlying medical conditions like HIV/AIDS, which directly attack immune cells. More commonly, it can be due to immunosuppressive medications used after an organ transplant or to treat autoimmune diseases like lupus or rheumatoid arthritis.
These medications work by intentionally dampening the immune response to prevent the body from rejecting an organ or attacking its own tissues. While essential for treating these conditions, a side effect is a reduced ability to control latent viruses like HPV. This is why individuals on these therapies are often monitored more closely for signs of HPV-related issues, as their risk of reactivation and progression to disease is higher.
Chronic Stress and Cortisol
The connection between mind and body is powerful, and chronic stress is a perfect example of how psychological state can impact physical health. When you experience prolonged stress—whether emotional, psychological, or physical—your body produces high levels of the hormone cortisol. While cortisol is useful in short-term "fight or flight" situations, sustained high levels can be detrimental to the immune system.
Cortisol suppresses the effectiveness of the immune system by lowering the number of lymphocytes (a type of white blood cell) and inhibiting communication between immune cells. This creates an environment where a dormant HPV infection can reawaken. Managing stress through techniques like mindfulness, exercise, adequate sleep, and therapy isn't just good for mental well-being; it's a crucial part of maintaining the immune strength needed to keep latent viruses at bay.
Smoking and Tobacco Use
Smoking is a major and well-documented risk factor for HPV activation and the progression to cervical cancer. The harmful chemicals in tobacco smoke have both local and systemic effects. Locally, in the cervix, these chemicals can damage the DNA of cervical cells and impair the function of specialized immune cells (like Langerhans cells) that are meant to fight off the virus in that tissue. This localized damage makes it easier for HPV to take hold and cause abnormal cell changes.
Systemically, smoking weakens the overall immune system, making it less efficient at fighting infections throughout the body. The combination of direct cellular damage and a weakened immune response creates a perfect storm for HPV to become active and persist, significantly increasing the risk of developing precancerous and cancerous lesions.
Co-infections with Other STIs
The presence of other sexually transmitted infections (STIs) can create an inflammatory environment in the genital tract that may trigger HPV reactivation. Infections like herpes, chlamydia, or gonorrhea cause the immune system to mount a strong, localized response. This inflammation, while intended to fight the new infection, can inadvertently create conditions that allow a dormant HPV virus to begin replicating again.
Furthermore, some STIs can cause sores or breaks in the skin, which can provide an easier entry point for new HPV infections or disrupt the cellular environment in a way that encourages a latent one to become active. Managing overall sexual health and getting regular screenings for all STIs is an important part of reducing the risk of HPV-related complications.
Hormonal Changes
Hormonal fluctuations, particularly involving estrogen and progesterone, can influence the cellular environment of the cervix and other tissues where HPV resides. This is why pregnancy is often associated with the appearance or growth of genital warts. The significant hormonal shifts and natural suppression of the immune system that occur during pregnancy can allow latent HPV to become active. In many cases, these warts resolve on their own after the baby is born and hormones return to normal levels.
Similarly, long-term use of hormonal contraceptives or hormonal changes associated with perimenopause and menopause can also impact the behavior of the virus. While the exact mechanisms are still being studied, it's believed that these hormones can influence viral gene expression, essentially helping to "turn on" the parts of the virus that lead to cell growth and replication.
Poor Nutrition and Vitamin Deficiencies
A balanced diet rich in vitamins and antioxidants is fundamental for a healthy immune system. Specific nutrient deficiencies have been linked to a reduced ability to control HPV. For example, vitamins like A, C, and E are powerful antioxidants that help protect cells from damage. B vitamins, particularly folate (B9), are essential for DNA repair and healthy cell division. A deficiency in folate has been associated with an increased risk of HPV persistence and cervical dysplasia.
Eating a diet full of fruits, vegetables, lean proteins, and whole grains provides the building blocks your immune system needs to function optimally. Conversely, a diet high in processed foods, sugar, and unhealthy fats can promote inflammation and weaken the body's defenses, potentially giving a dormant virus the upper hand.