Understanding 3 Common Pacemaker Side Effects: What Patients Should Know
Getting a pacemaker is a major step toward better heart health, and a key part of the process is knowing what to expect during recovery. While the procedure is overwhelmingly successful, being prepared for potential side effects can help you feel more confident and in control.
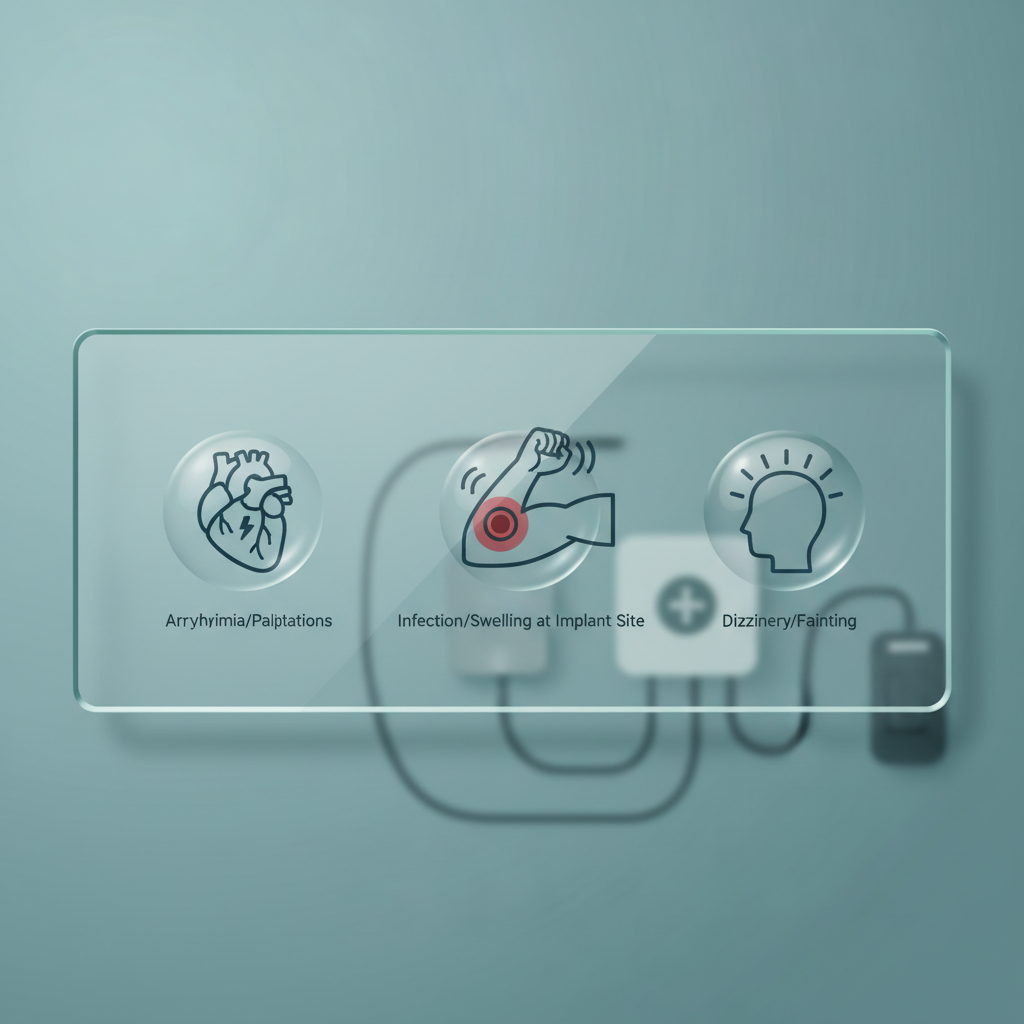
3 Pacemaker Side Effects Patients Should Prepare For
Receiving a pacemaker can be a life-changing and often life-saving event for individuals with certain heart rhythm disorders. This small electronic device helps regulate the heartbeat, ensuring it doesn't beat too slowly. While the procedure is common and generally safe, like any medical intervention, it comes with potential side effects. Being informed about these possibilities is a crucial part of the preparation and recovery process. Awareness allows patients and their families to recognize potential issues early and seek timely medical advice.
Understanding these side effects isn't meant to cause alarm, but rather to empower you with knowledge. Knowing what to look for can help you distinguish between normal post-operative healing and a complication that requires attention. Here, we'll explore three key side effects that patients should be prepared for after receiving a pacemaker.
1. Infection at the Implant Site
One of the most significant risks following any surgical procedure, including pacemaker implantation, is infection. The incision site where the pulse generator is placed (usually in the upper chest) is a potential entry point for bacteria. While doctors take extensive precautions to maintain a sterile environment during the surgery, infections can still occur in the days or even weeks following the procedure. Recognizing the signs early is critical to preventing the infection from spreading or becoming more serious.
Symptoms of an infection at the implant site include increasing redness, swelling, or warmth around the incision. You might also notice drainage or pus from the wound, experience a fever, or feel increased pain that isn't managed by prescribed medication. It is absolutely crucial not to dismiss these signs as a normal part of healing. If you notice any of these symptoms, you should contact your doctor's office immediately. Treatment typically involves antibiotics, and in more severe cases, it may require a procedure to clean the area or even remove and replace the pacemaker system.
2. Hematoma or Excessive Bruising
A hematoma is a collection of blood that pools outside of the blood vessels, essentially a deep and significant bruise. It's common to have some bruising around the pacemaker implant site after surgery, but a large, swollen, and firm hematoma is a complication that needs monitoring. This occurs when a blood vessel is nicked during the procedure and continues to leak blood into the surrounding tissue. Patients who take blood-thinning medications are at a slightly higher risk for developing a hematoma.
While a small hematoma might resolve on its own over time, a large one can be very painful and put pressure on the pacemaker device and the skin. In rare cases, a large, expanding hematoma may require medical intervention to drain the collected blood and relieve the pressure. You should watch for bruising that seems to be growing in size, significant swelling that makes the area feel tight and hard, or pain that worsens instead of improving after the first few days. Informing your care team about these symptoms will allow them to assess the situation and decide on the best course of action.
3. Pacemaker Malfunction and "Pacemaker Syndrome"
Although modern pacemakers are incredibly reliable, malfunctions can happen. This can involve issues with the battery, the leads (the wires connecting the device to the heart), or the pulse generator itself. One specific issue is called "pacemaker syndrome," which occurs when the timing of the pacing between the heart's upper and lower chambers is out of sync. This can cause blood to be pumped inefficiently, leading to a collection of uncomfortable symptoms.
Symptoms of a potential pacemaker malfunction or pacemaker syndrome can mirror the very symptoms the device was meant to treat. These include dizziness, fainting or near-fainting spells, shortness of breath, fatigue, and palpitations (a feeling of a pounding or fluttering heart). You might also experience swelling in your legs or abdomen. It's vital to remember that these devices are programmed specifically for your needs, and sometimes adjustments are required after the initial implantation. If you experience a return of your pre-pacemaker symptoms, contact your cardiologist. They can interrogate the device non-invasively to check its function and make programming changes to resolve the issue.
Understanding the Role of a Pacemaker
To fully appreciate the context of these side effects, it helps to understand what a pacemaker does and why it's needed. The human heart has its own natural electrical system that controls the rate and rhythm of its beats. When this system malfunctions, it can lead to arrhythmias, or irregular heartbeats. A pacemaker is prescribed when the heart beats too slowly, a condition known as bradycardia, or when the electrical signals are blocked, a condition called a heart block.
A pacemaker system consists of two main parts: the pulse generator and the leads. The pulse generator is a small metal case containing a battery and the tiny computer that regulates the heartbeat. It's typically implanted under the skin in the upper chest. The leads are thin, insulated wires that are threaded through a vein into the heart muscle. These leads deliver the electrical pulses from the generator to the heart, prompting it to beat at a normal rate. The device constantly monitors the heart's natural rhythm and will only send a signal when it detects that the beat is too slow or irregular. This "on-demand" function helps conserve battery life and allows the heart to beat on its own whenever it can.
Common Questions Patients Have After Pacemaker Surgery
What Are the Long-Term Lifestyle Adjustments with a Pacemaker?
Living with a pacemaker is often described as a "new normal." For the most part, patients can return to all their previous activities once they have fully recovered from the implantation surgery. However, there are a few key lifestyle adjustments and precautions to keep in mind. For the first few weeks, you'll likely be advised to limit heavy lifting and avoid raising the arm on the side of the implant above your shoulder to allow the leads to securely embed in the heart tissue.
In the long term, most household appliances and electronic devices are perfectly safe to use. The main concern is with devices that have strong magnetic or electromagnetic fields. You should keep cell phones and headphones at least six inches away from your pacemaker device—for example, by holding your phone to the ear on the opposite side of your body. You'll also need to inform security staff at airports or other venues with metal detectors that you have a pacemaker, as you should not go through the detector. Most daily activities, including exercise, driving, and hobbies, can be fully resumed based on your doctor's guidance.
How is a Pacemaker Monitored and Maintained?
A pacemaker isn't a "set it and forget it" device. It requires regular monitoring to ensure it is functioning correctly and that the battery life is sufficient. Your cardiology team will schedule regular follow-up appointments, often called "device checks." During these appointments, a special wand connected to a programmer is placed over your chest. This allows the doctor or technician to communicate with your pacemaker non-invasively to check its settings, review its performance history, and assess the remaining battery life.
Many modern pacemakers also come with remote monitoring capabilities. A small transmitter is kept in your home, usually by your bedside, which automatically collects data from your pacemaker and sends it to your doctor's office over a secure network. This allows your care team to monitor your device's function more frequently without you needing to come in for an in-person visit. Pacemaker batteries last for many years (typically 7 to 10 years or more), and when the battery gets low, you will need a relatively minor outpatient procedure to replace the pulse generator.
Conclusion
Getting a pacemaker is a significant step towards managing a heart rhythm disorder and improving your quality of life. While the technology is advanced and the procedure is generally very safe, being aware of potential side effects is a key part of the journey. Recognizing the signs of an infection, hematoma, or device malfunction enables you to seek prompt medical care, ensuring any issues are addressed quickly and effectively. By working closely with your healthcare team and understanding what to expect during recovery and beyond, you can confidently navigate life with your new device.
For more detailed information from trusted sources, please visit: