Understanding Skin Conditions That May Resemble HIV Rash
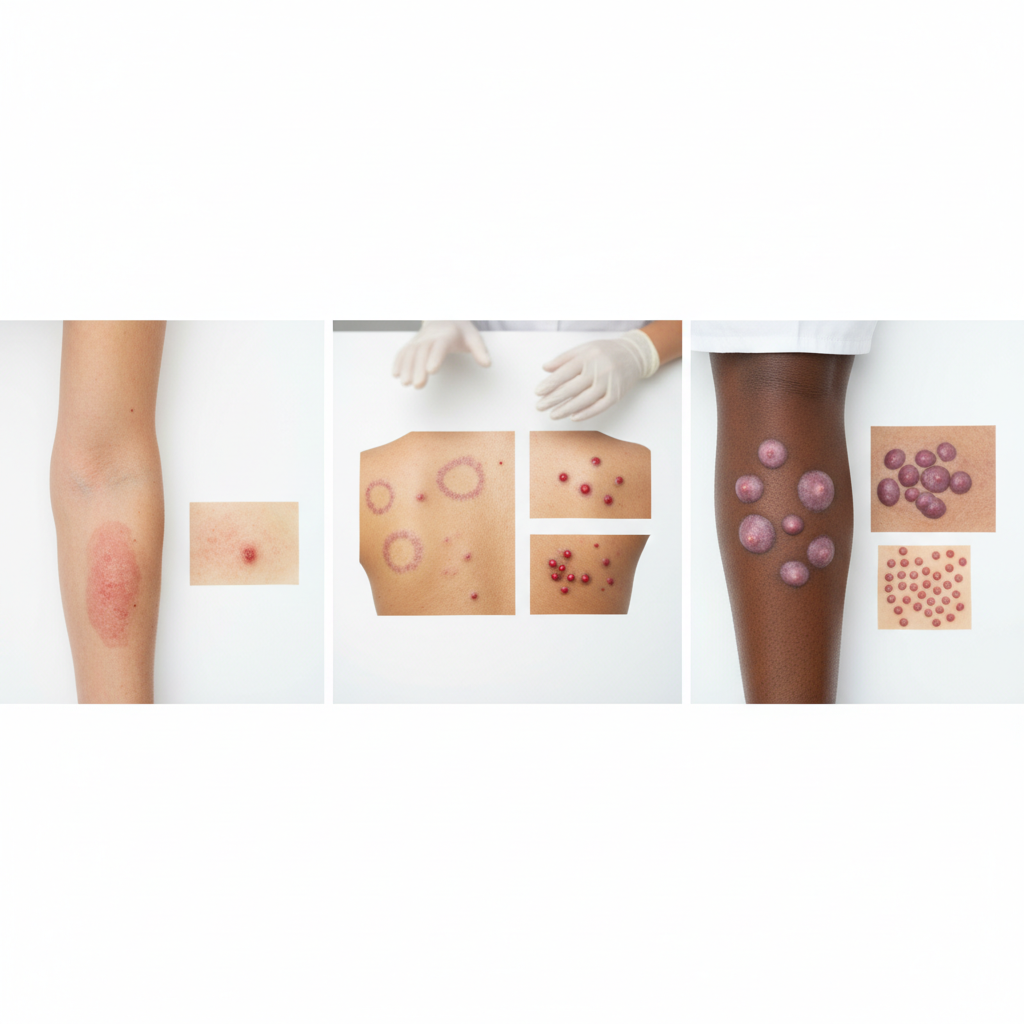
It’s understandable to feel concerned when a new, unfamiliar rash appears. While an HIV rash has distinct characteristics, several other common skin conditions—like pityriasis rosea, eczema, and even simple drug allergies—can look strikingly similar at first glance.
Skin Conditions That Can Resemble an HIV Rash
Navigating the world of skin conditions can be confusing and often stressful, especially when a new rash appears. One common concern is whether a rash could be a sign of HIV. While an acute HIV infection can indeed cause a rash, it's crucial to understand that many other, more common conditions can produce rashes that look very similar. Misidentification is frequent, leading to unnecessary anxiety. This guide provides a detailed look at various skin conditions that can mimic an HIV rash, helping you understand the different possibilities. However, it is essential to remember that only a qualified healthcare professional can provide an accurate diagnosis.
Pityriasis Rosea
Pityriasis rosea is a common skin condition that causes a temporary rash of raised, red, scaly patches on the body. It often begins with a single, larger oval patch called the "herald patch," which can be mistaken for ringworm. Within a week or two, smaller patches typically appear on the chest, back, and abdomen, often in a distinctive "Christmas tree" pattern. The rash can be itchy and is most common in older children and young adults.
The individual spots of pityriasis rosea can look similar to the maculopapular rash seen in acute HIV, which consists of flat, red areas with small, raised bumps. However, the presence of a herald patch and the specific Christmas tree distribution are key features that help differentiate it. While the exact cause of pityriasis rosea is unknown, it is thought to be triggered by a viral infection (not HIV) and usually resolves on its own within 6 to 8 weeks without treatment.
Drug Eruptions (Allergic Reactions)
A drug eruption is an adverse reaction to a medication, and it is one of the most common mimics of an HIV rash. These rashes can appear within days or even weeks of starting a new medication. The most frequent type is a morbilliform (measles-like) rash, which presents as widespread, symmetrical red macules and papules on the trunk and limbs. This appearance is almost identical to the rash associated with acute HIV seroconversion, making it a primary point of confusion.
Many different drugs can cause this reaction, including antibiotics (like penicillin and sulfa drugs), anti-seizure medications, and even over-the-counter pain relievers. The key to diagnosis is timing and medical history. If a rash develops shortly after starting a new medication, a drug eruption is a strong possibility. The rash typically resolves once the offending drug is discontinued, though a doctor should always be consulted before stopping any prescribed medication.
Secondary Syphilis
Syphilis, a sexually transmitted infection (STI) caused by the bacterium Treponema pallidum, can cause a skin rash in its secondary stage. This rash can vary greatly in appearance but often presents as rough, reddish-brown spots on the palms of the hands and the soles of the feet. This specific location is a classic sign of secondary syphilis and is less common with an HIV rash. However, the rash can also appear on other parts of the body, like the trunk, and can look like small, scaly macules or papules, leading to potential confusion.
Because both HIV and syphilis are STIs, co-infection is possible, and the risk factors are similar. The secondary syphilis rash may be accompanied by other symptoms like fever, sore throat, swollen lymph nodes, and patchy hair loss, which also overlap with symptoms of acute HIV. A definitive diagnosis requires a blood test specifically for syphilis, which is crucial for receiving appropriate antibiotic treatment.
Eczema (Atopic Dermatitis)
Eczema is a chronic inflammatory skin condition characterized by dry, itchy, and inflamed skin. While it often begins in childhood, it can persist or appear in adulthood. An eczema flare-up can cause red, bumpy, and scaly patches that can sometimes be mistaken for other rashes. The intense itching associated with eczema is a prominent feature, which may be less pronounced in an early HIV rash.
The location of the rash can also be a clue. Eczema commonly affects the "flexural" areas, such as the insides of the elbows and the backs of the knees. However, it can appear anywhere on the body. In individuals with darker skin, eczema may appear as grayish, brown, or purplish patches. A history of allergies or asthma often accompanies a diagnosis of eczema, which helps distinguish it from an acute viral rash.
Psoriasis
Psoriasis is a chronic autoimmune condition that accelerates the life cycle of skin cells, causing them to build up rapidly on the skin's surface. This results in thick, red, scaly patches called plaques, which are often covered with silvery scales. While classic plaque psoriasis looks distinct, other forms, like guttate psoriasis, can cause small, red, teardrop-shaped spots to appear suddenly over the trunk and limbs. This form is often triggered by a bacterial infection, like strep throat, and can be confused with a viral rash.
The thick, silvery scales are a hallmark of psoriasis that are not typically seen with an acute HIV rash. Psoriasis also tends to affect the scalp, elbows, and knees. It's important to note that HIV can sometimes trigger or worsen pre-existing psoriasis, but the rash itself is due to the autoimmune condition, not the virus directly.
Infectious Mononucleosis (Mono)
Often called the "kissing disease," infectious mononucleosis is caused by the Epstein-Barr virus (EBV). The symptoms of mono and acute HIV are remarkably similar: fever, fatigue, sore throat, and swollen lymph nodes. Mono can also cause a faint, pinkish, measles-like rash, particularly if the person is treated with certain antibiotics like amoxicillin or ampicillin while they have the infection.
Because the systemic symptoms overlap so closely, differentiating between mono and acute HIV based on symptoms alone is nearly impossible. Both are viral illnesses that cause the body to react in similar ways. Therefore, if a person presents with these symptoms and a rash, blood tests are essential to distinguish between EBV and HIV to ensure an accurate diagnosis and appropriate management.
Scabies
Scabies is an intensely itchy skin condition caused by a tiny burrowing mite called Sarcoptes scabiei. The primary symptom is severe itching that is usually worse at night. The rash itself consists of tiny red bumps, blisters, and sometimes thin, wavy lines (burrows) where the mites have tunneled into the skin. It commonly appears in the webbing between fingers, on the wrists, elbows, armpits, and along the waistline.
While the rash of scabies can look like a generic red, bumpy rash, the defining characteristic is the unrelenting itch. This level of itchiness is not typically the primary complaint with an early HIV rash. Additionally, scabies is highly contagious through prolonged skin-to-skin contact, so a history of close contact with an infected person can be a major clue. Diagnosis is often confirmed by a doctor identifying a mite burrow or examining a skin scraping under a microscope.
Understanding the Typical HIV Rash
To understand why so many conditions can mimic an HIV rash, it helps to know what doctors look for in a rash associated with acute HIV infection. This rash, also known as an acute retroviral syndrome (ARS) or seroconversion rash, typically appears 2 to 4 weeks after initial exposure to the virus. It occurs in a significant percentage of people who are newly infected as their body begins to mount an immune response.
The classic HIV rash is described as maculopapular. "Macules" are flat, discolored spots, and "papules" are small, raised bumps. The rash is usually red or reddish-brown and is not typically itchy or painful, although some people may experience mild itching. It most commonly appears on the upper body—primarily the trunk, chest, and face—but can also spread to the limbs, including the palms and soles. A key feature is that this rash is almost always accompanied by other flu-like symptoms, such as fever, fatigue, sore throat, headache, muscle aches, and swollen lymph nodes. The rash itself usually lasts for one to two weeks before resolving on its own.
Common Questions About Identifying Rashes
When Should You See a Doctor About a Rash?
It's always a good idea to consult a healthcare professional for any new, unexplained rash, especially if it's accompanied by other symptoms. Self-diagnosis can lead to anxiety and improper treatment. You should seek prompt medical attention if your rash is widespread, appears suddenly and spreads rapidly, is painful, or shows signs of infection like pus, swelling, or warmth.
Furthermore, if a rash is accompanied by systemic symptoms like fever, difficulty breathing, joint pain, or significant fatigue, a medical evaluation is critical. These can be signs of a more serious underlying condition, including a viral infection, a severe allergic reaction, or an autoimmune disease. A doctor can assess your complete symptom profile and medical history to determine the cause.
How Are These Rashes Diagnosed?
Diagnosing a rash involves a multi-step process. A doctor will start with a physical examination, looking at the rash's appearance, texture, and distribution on your body. They will ask detailed questions about when the rash started, whether it itches or hurts, any recent changes in your life (like starting new medications), your travel history, and any accompanying symptoms.
In many cases, a diagnosis can be made based on this initial evaluation. However, if the cause is unclear, further testing may be required. This can include blood tests to check for infections (like HIV, syphilis, or EBV) or markers of inflammation. In some instances, a doctor might perform a skin biopsy, where a small sample of the affected skin is removed and examined under a microscope to identify the underlying cause.
Can Stress Cause a Rash That Looks Like an HIV Rash?
Yes, stress can be a significant trigger for various skin conditions. While stress itself does not cause HIV, it can provoke rashes that might cause concern. The most common stress-induced rashes are hives (urticaria) and flare-ups of chronic conditions like eczema or psoriasis. Hives appear as raised, itchy welts that can vary in size and may come and go quickly.
A stress-induced eczema flare can result in red, itchy, and inflamed patches of skin. Because stress weakens the immune system, it can make the body more susceptible to skin issues. While these rashes can be red and bumpy, they often have distinguishing features, such as the intense itchiness of hives or the characteristic dry, scaly patches of eczema. However, because anxiety about HIV can itself be a source of stress, it can create a cycle where worry leads to a rash, which in turn leads to more worry.
Conclusion
A skin rash can be a symptom of many different health issues, ranging from minor allergic reactions to more serious infections. While an acute HIV infection can cause a distinct maculopapular rash, numerous other conditions—including pityriasis rosea, drug eruptions, secondary syphilis, and mono—can present with very similar appearances. Key differentiating factors often include the presence of other unique signs (like a herald patch or sores on the palms), the timing of the rash in relation to new medications, and the presence or absence of severe itching. Ultimately, the only way to confirm or rule out HIV is through testing. If you have a new, unexplained rash, especially if it is accompanied by flu-like symptoms, seeking a timely and accurate diagnosis from a healthcare professional is the most important step you can take for your health and peace of mind.