Understanding the Causes of Colon Inflammation
Colon inflammation, or colitis, isn't caused by just one thing; it's a symptom with a wide range of potential triggers. These can vary from temporary problems like bacterial infections and food sensitivities to chronic autoimmune conditions such as Crohn's disease and ulcerative colitis.
The Primary Causes of Colon Inflammation
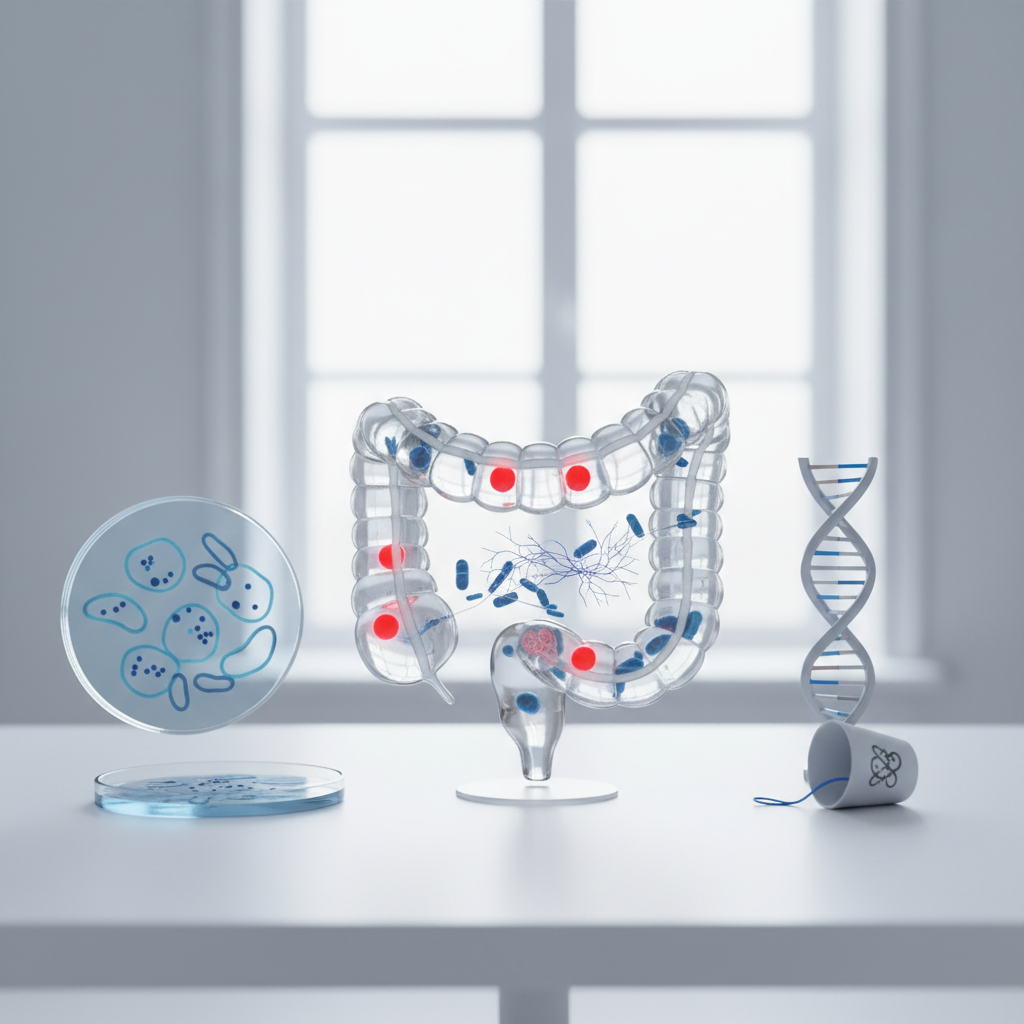
Colon inflammation, medically known as colitis, is a condition where the inner lining of the colon (the large intestine) becomes swollen, irritated, and inflamed. This condition can range from mild and temporary to severe and chronic, significantly impacting a person's quality of life. Understanding the root cause is the first step toward proper management. The causes are diverse, stemming from autoimmune disorders, infections, and even external factors like medication or medical treatments.
Below, we explore the most common culprits behind an inflamed colon, each with its own unique characteristics and mechanisms.
1. Inflammatory Bowel Disease (IBD)
Inflammatory Bowel Disease is a broad term for two primary chronic conditions characterized by long-term inflammation of the digestive tract: Ulcerative Colitis and Crohn's Disease. These are autoimmune conditions, meaning the body's immune system mistakenly attacks its own healthy tissues. In IBD, the target is the gastrointestinal (GI) tract. While the exact cause of this immune malfunction is unknown, it's believed to be a combination of genetic predisposition and environmental triggers.
Ulcerative Colitis (UC) specifically affects the colon and rectum. The inflammation is continuous and confined to the innermost lining of the colon. It almost always begins in the rectum and can spread upward to involve the entire colon. Crohn's Disease, on the other hand, can affect any part of the GI tract, from the mouth to the anus. The inflammation in Crohn's is often patchy, with healthy tissue interspersed between inflamed areas, and it can penetrate deeper into the layers of the bowel wall.
2. Infections (Infectious Colitis)
Sometimes, colon inflammation is a direct result of an infection from a harmful microorganism. This is known as infectious colitis and is often acute, meaning it comes on suddenly and typically resolves once the infection is treated. Several types of pathogens can be responsible for this condition.
Common culprits include bacteria like Clostridioides difficile (often called C. diff), which can overgrow after a course of antibiotics, as well as foodborne bacteria such as Salmonella, E. coli, and Campylobacter. Viruses, like Cytomegalovirus (CMV), can also cause colitis, particularly in individuals with compromised immune systems. Additionally, certain parasites, such as Entamoeba histolytica, can invade the colon and trigger significant inflammation.
3. Ischemic Colitis
Ischemic colitis occurs when blood flow to a part of the colon is temporarily reduced or blocked. Just like any other organ, the colon needs a steady supply of oxygen-rich blood to function properly. When this supply is compromised, the tissues can become damaged and inflamed. This condition is more common in older adults, as the risk factors are often related to cardiovascular health.
The reduction in blood flow can be caused by several factors. Atherosclerosis, or the hardening and narrowing of the arteries, is a common cause. A blood clot that travels to an artery supplying the colon can also create a blockage. Other potential causes include extremely low blood pressure (often due to shock or dehydration), bowel obstruction, or complications from certain surgeries.
4. Microscopic Colitis
As the name suggests, microscopic colitis is a type of inflammation that is not visible to the naked eye during a standard colonoscopy. A diagnosis can only be made by examining a tissue sample (biopsy) from the colon under a microscope. While its exact cause is not fully understood, it is thought to be an immune-related issue, potentially triggered by medications or bacteria.
There are two main subtypes of microscopic colitis. Lymphocytic colitis is characterized by an increased number of white blood cells (lymphocytes) in the lining of the colon. Collagenous colitis is identified by a thickened layer of collagen (a structural protein) just beneath the colon's lining. Both types primarily cause chronic, watery, non-bloody diarrhea.
5. Medication-Induced Colitis
Certain medications can irritate the lining of the colon and lead to inflammation. The most well-known offenders are nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen. While these are common over-the-counter pain relievers, long-term or high-dose use can damage the GI tract, leading to ulcers and inflammation.
Other medications can also be responsible. Some chemotherapy drugs, certain antibiotics that disrupt the gut's natural bacterial balance, and even some heart medications have been linked to colitis in susceptible individuals. It's crucial to discuss any new or worsening digestive symptoms with a doctor, especially if they coincide with starting a new medication.
6. Radiation Colitis
This form of colitis is a side effect of radiation therapy used to treat cancers in the pelvic or abdominal area, such as cervical, prostate, or rectal cancer. The radiation, while effective at targeting cancer cells, can also inadvertently damage the healthy cells of the nearby colon. This damage can lead to inflammation, ulcers, and scarring.
Radiation colitis can manifest in two ways. Acute radiation colitis occurs during or shortly after the treatment course and often resolves within a few weeks. Chronic radiation colitis, however, can develop months or even years after the therapy has concluded and may cause long-term problems due to permanent changes in the colon tissue.
Understanding the Colon's Role in Your Body
To fully appreciate why colon inflammation is so disruptive, it helps to understand what the colon does. The colon, also known as the large intestine, is the final part of the digestive tract. It's a long, muscular tube that connects the small intestine to the rectum. Its primary job isn't to digest food—that's mostly done in the small intestine—but to process what's left over.
The main function of the colon is to absorb water and electrolytes (like sodium and potassium) from the remaining indigestible food matter. This process is crucial for maintaining the body's fluid balance and solidifying waste into stool. The colon is also home to trillions of beneficial bacteria, collectively known as the gut microbiome. These bacteria play a vital role in synthesizing certain vitamins, breaking down fiber, and supporting the immune system. When the colon becomes inflamed, all of these critical functions can be impaired, leading to the characteristic symptoms of colitis.
Common Questions About Colon Health
What are the common symptoms of an inflamed colon?
While the underlying cause of colitis can vary, many of the symptoms are shared across the different types. The most common sign is a change in bowel habits. This often includes persistent diarrhea, which may be watery or contain blood, mucus, or pus. Abdominal pain, cramping, and bloating are also very common, as the inflamed tissues become sensitive and irritated.
Another frequent symptom is a feeling of urgency—an intense and sudden need to have a bowel movement. Some people may also experience tenesmus, which is the sensation of needing to pass stools even when the bowel is empty. Beyond digestive symptoms, chronic inflammation can take a toll on the entire body, leading to fatigue, unexplained weight loss, fever, and a general feeling of being unwell.
How is colon inflammation diagnosed?
Diagnosing colitis requires a thorough investigation to identify the specific cause and extent of the inflammation. The process typically begins with a healthcare provider taking a detailed medical history and performing a physical exam. From there, several tests may be ordered to get a clearer picture of what's happening inside the colon.
Blood tests can reveal signs of inflammation (like elevated C-reactive protein), anemia from blood loss, or infection. Stool samples are analyzed to rule out infectious causes by looking for bacteria, parasites, or toxins like C. diff. The most definitive diagnostic tool is often a colonoscopy. During this procedure, a doctor uses a thin, flexible tube with a camera to directly view the entire lining of the colon. This allows them to see the extent of the inflammation and take small tissue samples (biopsies) for microscopic analysis, which is essential for diagnosing conditions like microscopic colitis.
Can diet and lifestyle affect colon inflammation?
Yes, diet and lifestyle can play a significant role in managing colon inflammation, although they are not typically the root cause of conditions like IBD. For many people with colitis, certain foods can act as triggers, worsening symptoms like cramping and diarrhea. Common triggers include spicy foods, high-fat foods, dairy, caffeine, alcohol, and foods high in insoluble fiber (like raw vegetables and nuts). Keeping a food diary can help identify personal trigger foods.
Lifestyle factors are also important. Chronic stress is known to exacerbate inflammation and can trigger symptom flare-ups in people with IBD. Finding healthy ways to manage stress, such as through exercise, meditation, or therapy, can be beneficial. Smoking is a major risk factor, particularly for Crohn's disease, and quitting can lead to significant improvement. Staying hydrated is also crucial, especially when experiencing diarrhea, to prevent dehydration.
Key Takeaways on Colon Inflammation
Colon inflammation is a complex issue with a wide array of potential causes, from chronic autoimmune diseases and infections to reactions to medications and medical treatments. While the symptoms can often be similar—including diarrhea, abdominal pain, and urgency—the underlying reason for the inflammation dictates the best course of action.
Because the causes are so diverse, obtaining an accurate diagnosis from a healthcare professional is essential. Through a combination of medical history, lab tests, and procedures like a colonoscopy, doctors can pinpoint the specific type of colitis and develop an appropriate management plan. Recognizing the symptoms and understanding the potential causes is the first step toward addressing this challenging but manageable condition.