Understanding the Early Signs of Congestive Heart Failure: Learn How to Identify and Act
Recognizing congestive heart failure early is crucial, but its initial symptoms are often subtle and easily mistaken for normal signs of aging.
Recognizing the Early Warning Signs of Congestive Heart Failure
Congestive heart failure (CHF) is a chronic condition where the heart muscle doesn't pump blood as well as it should. When this happens, blood often backs up, and fluid can build up in the lungs and other parts of the body. Recognizing the early signs is crucial for managing the condition effectively. It's important to note that these symptoms can also be related to other health issues, so a proper medical evaluation is always necessary for a diagnosis. The following are some of the most common early indicators.
1. Shortness of Breath (Dyspnea)
One of the hallmark signs of early congestive heart failure is shortness of breath, medically known as dyspnea. This can occur during physical activity, while you are at rest, or even when you're lying flat in bed. When the heart can't pump efficiently, blood can back up in the pulmonary veins (the vessels that carry blood from the lungs to the heart), causing fluid to leak into the lungs. This condition, called pulmonary edema, makes it difficult for oxygen to move through the air sacs, leading to a feeling of breathlessness.
In the initial stages, you might only notice this after moderate exertion, like climbing a flight of stairs or carrying groceries. As the condition progresses, you might find yourself needing to prop your head up with several pillows to breathe comfortably at night (orthopnea) or waking up suddenly feeling like you're suffocating (paroxysmal nocturnal dyspnea).
2. Persistent Coughing or Wheezing
A chronic cough or wheezing that produces white or pink blood-tinged phlegm can be another sign of fluid accumulation in the lungs due to heart failure. This is often mistaken for asthma, bronchitis, or a lingering cold. However, in the context of CHF, this "cardiac cough" is a direct result of the fluid buildup irritating the airways.
The cough may worsen when you lie down or after you’ve been sleeping for a few hours. Unlike a respiratory infection, this type of cough doesn't typically come with a fever or other signs of illness. If you have a persistent, nagging cough that doesn't seem to have a clear cause, it’s a symptom worth discussing with a healthcare professional.
3. Swelling in Legs, Ankles, and Feet (Edema)
When the heart's pumping power is diminished, it can affect blood flow throughout the body. The right side of the heart, in particular, pumps blood to the lungs, but when it weakens, it can cause blood to back up in the veins. This increased pressure can force fluid out of the blood vessels and into the surrounding tissues, a condition known as edema. This swelling is most noticeable in the lower extremities—the legs, ankles, and feet—due to the effects of gravity.
You might notice that your shoes feel tighter than usual or that pressing a finger into your skin leaves a temporary indentation (pitting edema). Swelling can also occur in the abdomen (ascites) or lead to noticeable weight gain from fluid retention.
4. Unexplained Fatigue and Weakness
Profound and persistent fatigue is a very common, yet often overlooked, early sign of heart failure. When the heart cannot pump enough oxygen-rich blood to meet the body's needs, it diverts blood away from less vital organs, like the muscles in your limbs, to supply the brain and heart. This leaves you feeling tired, weak, and with a general lack of energy.
Everyday activities that were once easy, such as walking, shopping, or doing household chores, may become exhausting. This isn't the normal tiredness you feel after a long day; it's a deep-seated fatigue that doesn't improve significantly with rest.
5. Rapid or Irregular Heartbeat (Palpitations)
To compensate for its inability to pump blood effectively, the heart may try to beat faster (tachycardia) to circulate more blood. This can lead to a sensation of a racing heart or palpitations, where you feel like your heart is skipping beats, fluttering, or pounding in your chest. These sensations can be unsettling and may occur even when you are at rest.
While an occasional palpitation can be normal, frequent or sustained periods of a rapid or irregular heartbeat could indicate that your heart is working overtime to compensate for a loss in pumping function, which is a key aspect of congestive heart failure.
6. Sudden or Rapid Weight Gain
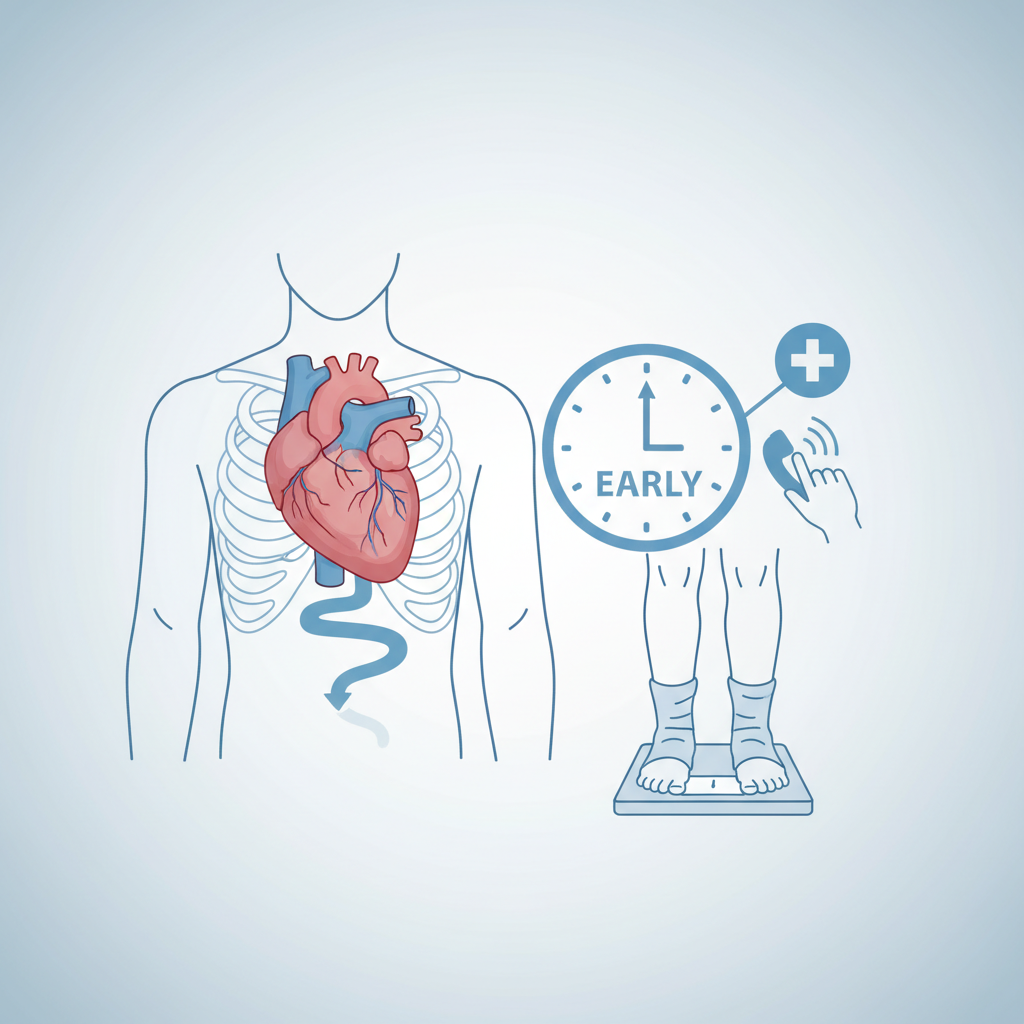
A rapid increase in weight—such as gaining two to three pounds in a 24-hour period or five pounds in a week—is often a red flag for fluid retention associated with worsening heart failure. This weight gain isn't from fat or muscle but from the body holding onto excess fluid. This fluid can accumulate in the lungs, abdomen, and lower limbs, leading to the swelling and shortness of breath previously mentioned.
Many healthcare providers advise patients with heart failure to weigh themselves daily at the same time, typically in the morning, to monitor for these sudden changes. It’s one of the most reliable ways to track fluid buildup before more severe symptoms appear.
7. Lack of Appetite or Nausea
When the digestive system receives less blood due to the heart's poor pumping function, it can lead to problems with digestion. This can manifest as a feeling of fullness even after eating very little, a general lack of appetite, or persistent nausea. The fluid buildup in the abdomen (ascites) can also put pressure on the stomach and intestines, further contributing to these feelings of discomfort and making it difficult to eat a full meal.
8. Difficulty Concentrating or Decreased Alertness
The brain needs a constant supply of oxygen-rich blood to function properly. In some cases of heart failure, reduced blood flow can affect cognitive function. This may lead to feelings of confusion, memory loss, disorientation, or difficulty concentrating. Family members are often the first to notice these subtle changes in a person's mental state. This symptom is sometimes referred to as "brain fog" and can be particularly noticeable in more advanced stages of the condition.
What Exactly Is Congestive Heart Failure?
It's a common misconception that "heart failure" means the heart has stopped working entirely. In reality, congestive heart failure (CHF) is a condition where the heart muscle has become weakened or stiff and cannot pump blood as efficiently as it should. The "failure" refers to the heart's inability to keep up with the body's demands for blood and oxygen.
The term "congestive" specifically refers to the stage where fluid backs up in various parts of the body. As the heart's pumping action becomes less effective, blood returning to the heart through the veins backs up, causing congestion in the body's tissues. This often results in fluid buildup in the lungs (pulmonary edema) and swelling in other areas like the legs and abdomen (peripheral edema). The condition can affect the right side, the left side, or both sides of the heart, with each causing a different set of primary symptoms.
Common Questions and Related Concerns About Heart Health
What Are the Primary Causes of Congestive Heart Failure?
Congestive heart failure is typically the end result of other conditions that have damaged or overworked the heart muscle over time. The most common cause is coronary artery disease (CAD), where narrowed arteries reduce blood flow to the heart muscle, leading to heart attacks that damage the tissue. Another major contributor is long-term high blood pressure (hypertension), which forces the heart to work harder to circulate blood, eventually causing the muscle to thicken and weaken.
Other conditions that can lead to heart failure include faulty heart valves, which disrupt normal blood flow; damage to the heart muscle from infections or alcohol use (cardiomyopathy); and uncontrolled diabetes, which increases the risk of both hypertension and CAD. Conditions like thyroid disease, severe anemia, and abnormal heart rhythms (arrhythmias) can also contribute to the development of CHF over time.
How Is Heart Failure Typically Diagnosed?
Diagnosing heart failure involves a multi-step process that starts with a thorough physical exam and a review of the patient's medical history and symptoms. A doctor will listen to the heart and lungs with a stethoscope to check for fluid (crackles) or abnormal heart sounds. They will also check for swelling in the legs, ankles, and abdomen.
To confirm a diagnosis and determine the underlying cause, several tests are commonly used. A blood test can check for levels of a hormone called B-type natriuretic peptide (BNP), which rises when the heart is under stress. An electrocardiogram (ECG or EKG) records the heart's electrical activity to detect rhythm problems or signs of a past heart attack. The most definitive diagnostic tool is often an echocardiogram, which uses sound waves to create a video image of the heart, showing its size, shape, and how well its chambers and valves are working. This test can measure the ejection fraction, a key indicator of the heart's pumping ability.
Can Lifestyle Changes Make a Difference in Heart Health?
Lifestyle modifications play a significant role in both managing existing heart conditions and reducing the risk of developing them in the first place. For individuals with or at risk for heart failure, making positive changes can significantly improve quality of life and slow the progression of the disease. A heart-healthy diet low in sodium is particularly important, as excess salt causes the body to retain fluid, putting extra strain on the heart.
Regular physical activity, as approved by a doctor, helps strengthen the heart muscle and improve circulation. Limiting or avoiding alcohol, quitting smoking, and managing stress are also crucial components of a heart-healthy lifestyle. Furthermore, effectively managing underlying conditions like high blood pressure, high cholesterol, and diabetes through medication and lifestyle changes is fundamental to protecting the heart from further damage.
Understanding the Importance of Early Recognition
Recognizing the early signs of congestive heart failure is the first step toward seeking a proper diagnosis and management plan. Symptoms like shortness of breath, fatigue, and swelling are the body's way of signaling that the heart is struggling to do its job. While these signs can be subtle at first, paying attention to them and discussing them with a healthcare provider can lead to earlier intervention. Understanding these indicators allows individuals to take a more proactive role in their cardiovascular health.
For more detailed information from trusted sources, you can visit: